Implantable Collamer Lens (ICL) Surgery
Visian ICL
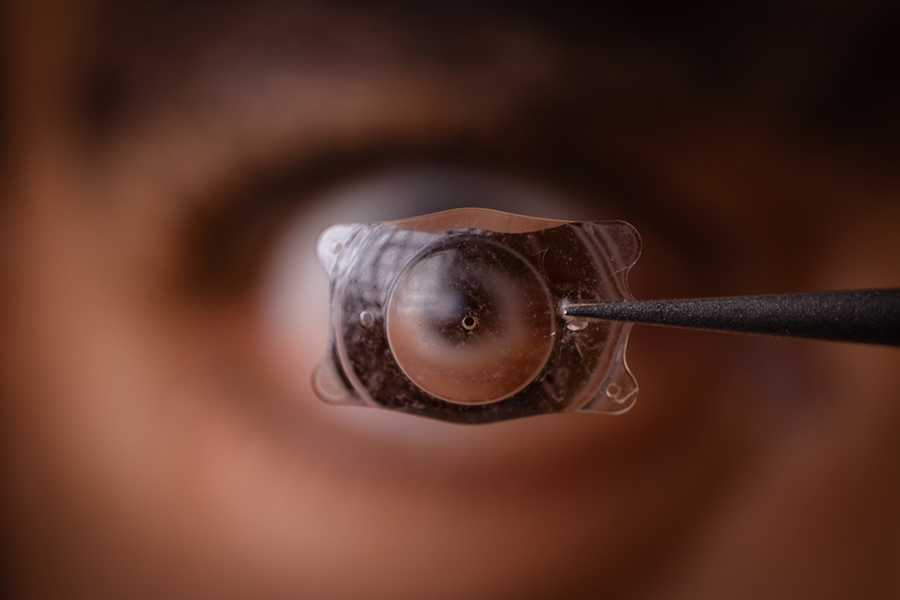
The most common technique to correct your eyes to be able to function without glasses utilizes the Excimer laser. In LASIK and PRK the surgeon reshapes the corneal tissue. Although the laser can treat a large range of prescriptions, there are still a significant number of individuals who are not candidates for these surgeries. Some patients have a prescription that is out of the treatable range, others have a thin cornea or an irregular corneal shape. In December 2005 the FDA approved a new surgery that can now help many of these patients. It is called the Visian ICL, or Implantable Collamer Lens.
How does the Visian ICL work?
The Visian ICL is made from a soft plastic and collagen-based material with a design similar to the existing intraocular lenses used to correct vision after cataract surgery. The ICL is placed through a small incision in the ey into the posterior chamber. It is designed to correct nearsightedness between -3 diopters and -15 diopters, and partially correct nearsightedness up to -20 diopters, with up to 2.5 diopters of astigmatism. It is permanent correction as long as the ICL is in the eye. The implant can be removed or replaced in the future if necessary. Although, the residual effect of the ICL on the eye after it is removed or replaced is unknown.
The Clinical Study to Evaluate Risk/Benefit of ICL
A clinical study of 526 eyes over 3 years was performed to determine benefits and risks of the implant. The study was then presented to the FDA in order to obtain approval to use the lens in the United States. The patients in the study ranged in age from 21 to 45 years old. The average amount of nearsightedness was -10.06 diopters, although the prescriptions ranged between -3 to -20.
Three years after insertion of the ICL, 94.7% of eyes saw 20/40 or better without glasses or contact lenses, 59.3% of these patients saw 20/20 or better. The patients that participated in the study were asked to report their satisfaction throughout the process, 92.1% of the patients expressed that they were very/extremely satisfied three years after the surgery, only 0.6% of cases were unsatisfied. The reported quality of vision reported as very good/excellent improved from 55% wearing glasses/contact lenses, to 77% with the implant, three years after the surgery.
The patients were also asked to rate worsened side effects 3 years after their surgery, the results were as follows; 9.7% of patients noted glare, 11.4% noted halos at night, 1.7% reported double vision, and 12% described night vision problems. Non of these patients felt that the symptoms were significant enough to warrant removal of the lens.
The insertion of the ICL is a surgical procedure, and carries potentially serious risks as with any surgery. The risks that were reported in this study were as follows:
Short term Complications included, removal and reinsertion of implant in 2.5%, need for enlargement of the peripheral iridectomy in 0.2%, and temporary swelling of the cornea 11.4%.
Complications after 1st week increase in astigmatism 0.4%, loss of best corrected vision 1.9%, clouding of the crystalline lens 1.4%, loss of cells from the back surface of the cornea responsible for the cornea remaining clear 8.9%, increase in eye pressure 0.4%, iris prolapse 0.2%, cloudy areas on the crystalline lens that may or may not cause patient symptoms 2.7%, macular hemorrhage 0.2%, retinal detachment 0.6%, secondary ICL related surgeries 3.1%, subretinal hemorrhage 0.2%, too much or too little nearsightedness correction 2%, additional YAG iridotomy necessary 3.2%.
Long term complications include clouding of the crystalline lens in 1.4% of patients, clouding of the crystalline lens not affecting vision in 2.7% of patients, enhancement to improve vision 2%, retinal detachment in 0.6% of patients and loss of cells on back of cornea in 8.9%.

What should I expect during the surgery?
Before your surgery, you will need to have a complete eye exam. Dr. Weisenthal will determine if your eyes are healthy and if you are a good candidate. If you are a contact lenses wearer you will need to leave the lenses out for the appropriate amount of time prior to your exam. You should have a stable prescription for at least one year prior to the exam. Once you have been approved by the doctor, the office will schedule you for a YAG iridotomy to prepare your eyes for the ICL. This procedure is performed 1-2 weeks prior to insertion of the ICL. The YAG iridotomy is necessary to ensure that the fluid flows properly from the back chamber to the front chamber of the ey to prevent a buildup of pressure within the eye after ICL surgery. This procedure only takes a few minutes, and doesn’t normally have any effect on vision.
The surgeries are performed in Liverpool at the Specialty Surgery Center. The day of the surgery you will be given dilation and numbing drops, and a mild sedative to relax you during the procedure. The surgery will take approximately 20-30 minutes or less. Dr. Weisenthal will make a small incision in your cornea, and insert the ICL. Once your procedure is complete we will explain your postoperative instructions, and Dr. Weisenthal will check you afterwards. Plan on being at the center for a few hours, and you will need to have a driver with you that day.
You will have an appointment in the office the day after your surgery to check your vision and eye pressure. You may be light sensitive for the first few days after your procedure. You may also experience some irritation in the eye during the healing process. After your surgery Dr. Weisenthal will prescribe antibiotics and anti-inflammatory eye drops to help with the healing of your eye. You may also notice some increase in dryness in the eye after your surgery, which can be treated using artificial tears, or a lubricating eye ointment.
Who is not a good candidate?
You should NOT have ICL surgery if you:
- Have narrow anterior chamber angle as determined by a special examination by your eye doctor, or if your doctor determines that the shape of your eye is not adequate to fit the ICL
- Are pregnant or nursing
- Do not meet the minimum endothelial cell density for your age at the time of implantation as determined by your eye doctor
Precautions:
- Patients with higher amounts of nearsightedness had worse results with lower effectiveness and higher risk of complications.
- The effect of pupil size on visual symptoms is not known.
- The relationship between the ICL and future lens opacities and retinal detachment is undetermined.
- There is currently is a lack of long-term data to assess cataract formation and cataract progression following removal and/or replacement of the lens.
- The effectiveness of ultraviolet absorbing lenses in reducing the incidence of retinal disorders has not been established.
- The safety and effectiveness of the ICL for the correction of moderate to high nearsightedness has not been established in patients:
- With unstable or worsening prescriptions
- With history or clinical signs of iritis/uveitis
- With diabetic retinopathy
- With glaucoma
- With history of previous eye surgery
- With serious (life-threatening) non-ophthalmic disease
- With progressive sight-threatening disease
- With a diagnosis of ocular-hypertension (high eye pressure)
- With insulin-dependent diabetes
- With pseudoexfoliation
- With pigment dispersion
- With greater than 20D of nearsightedness/2.5D of astigmatism